Overview
Within This Page
"A functional design can promote skill, economy, conveniences, and comforts; a non-functional design can impede activities of all types, detract from quality of care, and raise costs to intolerable levels." ... Hardy and Lammers
Hospitals are the most complex of building types. Each hospital is comprised of a wide range of services and functional units. These include diagnostic and treatment functions, such as clinical laboratories, imaging, emergency rooms, and surgery; hospitality functions, such as food service and housekeeping; and the fundamental inpatient care or bed-related function. This diversity is reflected in the breadth and specificity of regulations, codes, and oversight that govern hospital construction and operations. Each of the wide-ranging and constantly evolving functions of a hospital, including highly complicated mechanical, electrical, and telecommunications systems, requires specialized knowledge and expertise. No one person can reasonably have complete knowledge, which is why specialized consultants play an important role in hospital planning and design. The functional units within the hospital can have competing needs and priorities. Idealized scenarios and strongly-held individual preferences must be balanced against mandatory requirements, actual functional needs (internal traffic and relationship to other departments), and the financial status of the organization.

VA Medical Center, Bay Pines, Florida
In addition to the wide range of services that must be accommodated, hospitals must serve and support many different users and stakeholders. Ideally, the design process incorporates direct input from the owner and from key hospital staff early on in the process. The designer also has to be an advocate for the patients, visitors, support staff, volunteers, and suppliers who do not generally have direct input into the design. Good hospital design integrates functional requirements with the human needs of its varied users.
The basic form of a hospital is, ideally, based on its functions:
- bed-related inpatient functions
- outpatient-related functions
- diagnostic and treatment functions
- administrative functions
- service functions (food, supply)
- research and teaching functions
Physical relationships between these functions determine the configuration of the hospital. Certain relationships between the various functions are required—as in the following flow diagrams.
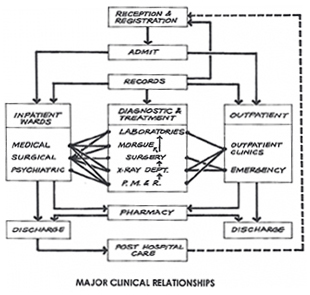
These flow diagrams show the movement and communication of people, materials, and waste. Thus the physical configuration of a hospital and its transportation and logistic systems are inextricably intertwined. The transportation systems are influenced by the building configuration, and the configuration is heavily dependent on the transportation systems. The hospital configuration is also influenced by site restraints and opportunities, climate, surrounding facilities, budget, and available technology. New alternatives are generated by new medical needs and new technology.
In a large hospital, the form of the typical nursing unit, since it may be repeated many times, is a principal element of the overall configuration. Nursing units today tend to be more compact shapes than the elongated rectangles of the past. Compact rectangles, modified triangles, or even circles have been used in an attempt to shorten the distance between the nurse station and the patient's bed. The chosen solution is heavily dependent on program issues such as organization of the nursing program, number of beds to a nursing unit, and number of beds to a patient room. (The trend, recently reinforced by HIPAA, is to all private rooms.)
Building Attributes
Regardless of their location, size, or budget, all hospitals should have certain common attributes.
Efficiency and Cost-Effectiveness
An efficient hospital layout should:
- Promote staff efficiency by minimizing distance of necessary travel between frequently used spaces
- Allow easy visual supervision of patients by limited staff
- Include all needed spaces, but no redundant ones. This requires careful pre-design programming.
- Provide an efficient logistics system, which might include elevators, pneumatic tubes, box conveyors, manual or automated carts, and gravity or pneumatic chutes, for the efficient handling of food and clean supplies and the removal of waste, recyclables, and soiled material
- Make efficient use of space by locating support spaces so that they may be shared by adjacent functional areas, and by making prudent use of multi-purpose spaces
- Consolidate outpatient functions for more efficient operation—on first floor, if possible—for direct access by outpatients
- Group or combine functional areas with similar system requirements
- Provide optimal functional adjacencies, such as locating the surgical intensive care unit adjacent to the operating suite. These adjacencies should be based on a detailed functional program which describes the hospital's intended operations from the standpoint of patients, staff, and supplies.
Flexibility and Expandability
Since medical needs and modes of treatment will continue to change, hospitals should:
- Follow modular concepts of space planning and layout
- Use generic room sizes and plans as much as possible, rather than highly specific ones
- Be served by modular, easily accessed, and easily modified mechanical and electrical systems
- Where size and program allow, be designed on a modular system basis, such as the VA Hospital Building System. This system also uses walk-through interstitial space between occupied floors for mechanical, electrical, and plumbing distribution. For large projects, this provides continuing adaptability to changing programs and needs, with no first-cost premium, if properly planned, designed, and bid. The VA Hospital Building System also allows vertical expansion without disruptions to floors below.
- Be open-ended, with well planned directions for future expansion; for instance positioning "soft spaces" such as administrative departments, adjacent to "hard spaces" such as clinical laboratories.
Cross-section showing interstitial space with deck above an occupied floor.
Therapeutic Environment
Hospital patients are often fearful and confused and these feelings may impede recovery. Every effort should be made to make the hospital stay as unthreatening, comfortable, and stress-free as possible. The interior designer plays a major role in this effort to create a therapeutic environment. A hospital's interior design should be based on a comprehensive understanding of the facility's mission and its patient profile. The characteristics of the patient profile will determine the degree to which the interior design should address aging, loss of visual acuity, other physical and mental disabilities, and abusiveness. (See VA Interior Design Manual.) Some important aspects of creating a therapeutic interior are:
- Using familiar and culturally relevant materials wherever consistent with sanitation and other functional needs
- Using cheerful and varied colors and textures, keeping in mind that some colors are inappropriate and can interfere with provider assessments of patients' pallor and skin tones, disorient older or impaired patients, or agitate patients and staff, particularly some psychiatric patients.
- Admitting ample natural light wherever feasible and using color-corrected lighting in interior spaces which closely approximates natural daylight
- Providing views of the outdoors from every patient bed, and elsewhere wherever possible; photo murals of nature scenes are helpful where outdoor views are not available
- Designing a "way-finding" process into every project. Patients, visitors, and staff all need to know where they are, what their destination is, and how to get there and return. A patient's sense of competence is encouraged by making spaces easy to find, identify, and use without asking for help. Building elements, color, texture, and pattern should all give cues, as well as artwork and signage. (As an example, see VA Signage Design Guide.)
For an in-depth view see WBDG Therapeutic Environments.
Cleanliness and Sanitation
Hospitals must be easy to clean and maintain. This is facilitated by:
- Appropriate, durable finishes for each functional space
- Careful detailing of such features as doorframes, casework, and finish transitions to avoid dirt-catching and hard-to-clean crevices and joints
- Adequate and appropriately located housekeeping spaces
- Special materials, finishes, and details for spaces which are to be kept sterile, such as integral cove base. The new antimicrobial surfaces might be considered for appropriate locations.
- Incorporating O&M practices that stress indoor environmental quality (IEQ)
Accessibility
VA Medical Center, Albuquerque, NM
All areas, both inside and out, should:
- Comply with the minimum requirements of the Americans with Disability Act (ADA) and, if federally funded or owned, the GSA's ABA Accessibility Standards
- In addition to meeting minimum requirements of ADA and/or GSA's ABA Accessibility Standards, be designed so as to be easy to use by the many patients with temporary or permanent handicaps
- Ensuring grades are flat enough to allow easy movement and sidewalks and corridors are wide enough for two wheelchairs to pass easily
- Ensuring entrance areas are designed to accommodate patients with slower adaptation rates to dark and light; marking glass walls and doors to make their presence obvious
Controlled Circulation
A hospital is a complex system of interrelated functions requiring constant movement of people and goods. Much of this circulation should be controlled.
- Outpatients visiting diagnostic and treatment areas should not travel through inpatient functional areas nor encounter severely ill inpatients
- Typical outpatient routes should be simple and clearly defined
- Visitors should have a simple and direct route to each patient nursing unit without penetrating other functional areas
- Separate patients and visitors from industrial/logistical areas or floors
- Outflow of trash, recyclables, and soiled materials should be separated from movement of food and clean supplies, and both should be separated from routes of patients and visitors
- Transfer of cadavers to and from the morgue should be out of the sight of patients and visitors
- Dedicated service elevators for deliveries, food and building maintenance services
Aesthetics
Aesthetics is closely related to creating a therapeutic environment (homelike, attractive.) It is important in enhancing the hospital's public image and is thus an important marketing tool. A better environment also contributes to better staff morale and patient care. Aesthetic considerations include:
- Increased use of natural light, natural materials, and textures
- Use of artwork
- Attention to proportions, color, scale, and detail
- Bright, open, generously-scaled public spaces
- Homelike and intimate scale in patient rooms, day rooms, consultation rooms, and offices
- Compatibility of exterior design with its physical surroundings
Security and Safety
In addition to the general safety concerns of all buildings, hospitals have several particular security concerns:
- Protection of hospital property and assets, including drugs
- Protection of patients, including incapacitated patients, and staff
- Safe control of violent or unstable patients
- Vulnerability to damage from terrorism because of proximity to high-vulnerability targets, or because they may be highly visible public buildings with an important role in the public health system.
Sustainability
Hospitals are large public buildings that have a significant impact on the environment and economy of the surrounding community. They are heavy users of energy and water and produce large amounts of waste. Because hospitals place such demands on community resources they are natural candidates for sustainable design.
Section 1.2 of VA's HVAC Design Manual is a good example of health care facility energy conservation standards that meet Energy Policy Act of 2005 (EPACT) and Executive Order 13693 requirements. The Energy Independence and Security Act of 2007 (EISA) provides additional requirements for energy conservation. Also see USGBC's Leadership in Energy and Environmental Design (LEED) for Healthcare.
Related Issues
The HIPAA (Health Insurance Portability and Accessibility Act of 1996) regulations address security and privacy of "protected health information" (PHI). These regulations put emphasis on acoustic and visual privacy, and may affect location and layout of workstations that handle medical records and other patient information, paper and electronic, as well as patient accommodations."
Emerging Issues
Among the many new developments and trends influencing hospital design are:
- The decreasing numbers of general practitioners along with the increased use of emergency facilities for primary care
- The increasing introduction of highly sophisticated diagnostic and treatment technology
- Requirements to remain operational during and after disasters—see, for example, VA's Physical Security Manuals
- State laws requiring earthquake resistance, both in designing new buildings and retrofitting existing structures
- Preventative care versus sickness care; designing hospitals as all-inclusive "wellness centers"
- Use of hand-held computers and portable diagnostic equipment to allow more mobile, decentralized patient care, and a general shift to computerized patient information of all kinds. This might require computer alcoves and data ports in corridors outside patient bedrooms. For more information, see WBDG Integrate Technological Tools
- Need to balance increasing attention to building security with openness to patients and visitors
- Emergence of palliative care as a specialty in many major medical centers
- A growing interest in more holistic, patient-centered treatment and environments such as promoted by Planetree. This might include providing mini-medical libraries and computer terminals so patients can research their conditions and treatments, and locating kitchens and dining areas on inpatient units so family members can prepare food for patients and families to eat together.
Relevant Codes and Standards
Hospitals are among the most regulated of all building types. Like other buildings, they must follow the local and/or state general building codes. However, federal facilities on federal property generally need not comply with state and local codes, but follow federal regulations. To be licensed by the state, design must comply with the individual state licensing regulations. Many states adopt the FGI Guidelines for Design and Construction of Health Care Facilities as a resource, and thus that volume often has regulatory status.
State and local building codes are based on the model ICC IBC International Building Code. Federal agencies are usually in compliance with the IBC except NFPA 101 (Life Safety Code), NFPA 70 (National Electric Code), and Architectural Barriers Act Accessibility Guidelines or GSA's ABA Accessibility Standards takes precedence.
Since hospitals treat patients who are reimbursed under Medicare, they must also meet federal standards, and to be accredited, they must meet standards of The Joint Commission. Generally, the federal government and The Joint Commission refer to the National Fire Protection Association (NFPA) model fire codes, including Standards for Health Care Facilities (NFPA 99) and the Life Safety Code (NFPA 101).
The Americans with Disabilities Act (ADA) applies to all public facilities and greatly affects the building design with its general and specific accessibility requirements. The Architectural Barriers Act Accessibility Guidelines or GSA's ABA Accessibility Standards apply to federal and federally funded facilities. The technical requirements do not differ greatly from the ADA requirements. See WBDG Accessible
Regulations of the Occupational Safety and Health Administration (OSHA) also affect the design of hospitals, particularly in laboratory areas.
Federal agencies that build and operate hospitals have developed detailed standards for the programming, design, and construction of their facilities. Many of these standards are applicable to the design of non-governmental facilities as well. Among them are:
- Department of Veterans Affairs (VA), Office of Construction & Facilities Management Technical Information Library contains many guides and standards, including Design Guides for planning many different departments and clinics, design manuals of technical requirements, equipment lists, master specifications, room finishes, space planning criteria, and standard details.
Federal Mandates and Criteria
- Executive Order 13693, "Planning for Federal Sustainability in the Next Decade"
- UFC 4-510-01 Design: Military Medical Facilities
Additional Resources
Publications
- Design Details for Health: Making the Most of Design's Healing Potential, 2nd Edition by Cynthia A. Leibrock and Debra Harris. New York: John Wiley & Sons, Inc., 2011. — Innovative design solutions in key areas such as lighting, acoustics, color, and finishes
- Design Guide for Improving Hospital Safety in Earthquakes, Floods, and High Winds: Providing Protection to People and Buildings. FEMA 577, 2007.
- Development Study—VA Hospital Building System: Application of the Principles of System Integration to the Design of VA Hospital Facilities Research Study Report Project Number 99-R047 by Building Systems Development and Stone, Marraccini & Patterson. Washington, DC: U.S. Government Printing Office, rev. 1977.
- Emergency Department Design: A Practical Guide to Planning for the Future. American College of Emergency Physicians (ACEP).
- Healthcare Facility Planning: Thinking Strategically, 2nd Edition by Cynthia Hayward, AIA, FAAHC, ACHA. Health Administration Press and the American College of Healthcare Executives, 2016.
- Hospitals, The Planning and Design Process, 2nd ed. by Owen B. Hardy and Lawrence P. Lammers. Rockville, Md.: Aspen Publishers, 1996.
- Hospital Interior Architecture: Creating Healing Environments for Special Patient Populations by Jain Malkin. New York: John Wiley & Sons, Inc., 1992.
- Healthcare Design — A quarterly magazine with design articles and presentations of recent projects
- Medical and Dental Space Planning: A Comprehensive Guide to Design, Equipment, and Clinical Procedures, 4th Edition, by Jain Malkin. New York: John Wiley & Sons, Inc., 2014.
- Sound & Vibration: Design Guidelines for Health Care Facilities by the Acoustics Research Council. 2010.
Tools
- SpaceMed Guide — A Space Planning Guide for Healthcare Facilities — a popular planning tool providing state-of-the-art planning methodologies, industry benchmarks, and planning tips.